Index Works
Vascular anomaly, venous malformation, sodium tetradecyl sulfate, sclerotherapy, embolization
Age & Gender
26-year-old female
Clinical findings
A 26-year-old female was referred to our institution for symptoms of pain, swelling, and decreased range of motion in her left forearm and wrist. The symptoms began at age 12 with menarche. She previously had an extensive workup for tendinitis, carpal tunnel syndrome, as well as other joint disorders. The patient had no significant past medical or surgical history. Physical examination demonstrated no thrill or bruit. The arm and wrist were normal in pallor and temperature when compared to the contralateral limb. Nail beds were pink with brisk capillary refill.
An MRI was performed at an outside institution (not shown), which demonstrated a slow- flow vascular malformation in the flexor digitorum superficialis muscle. The patient was referred for further evaluation and treatment.
Diagnosis
Venous malformation of the left flexor digitorum superficialis
Imaging Findings
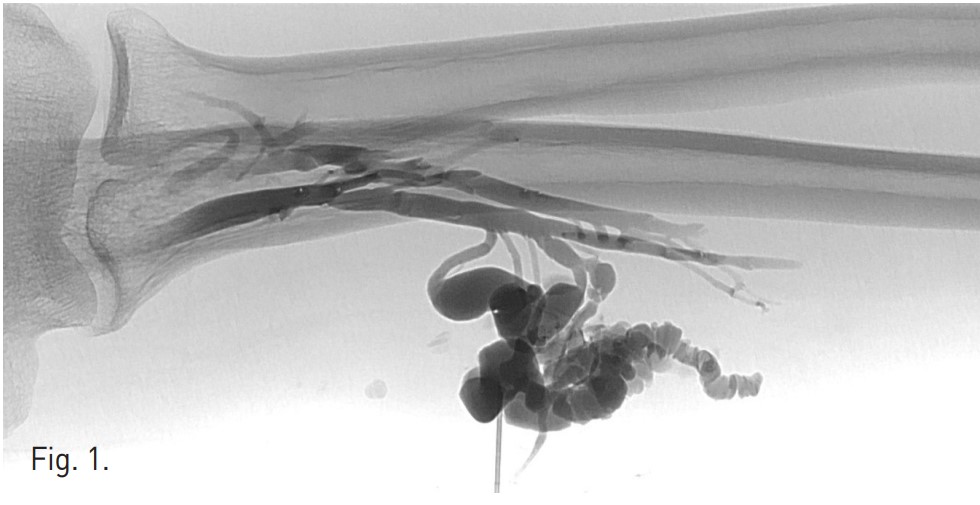
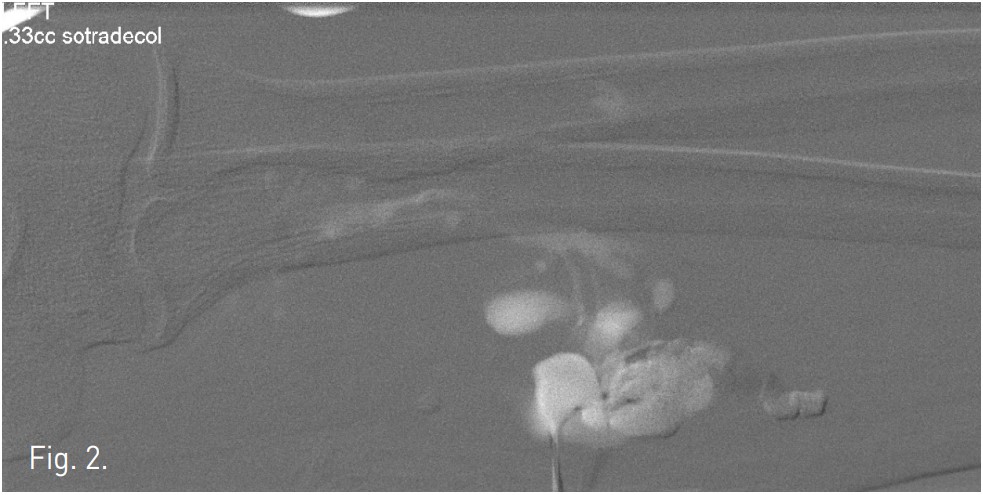
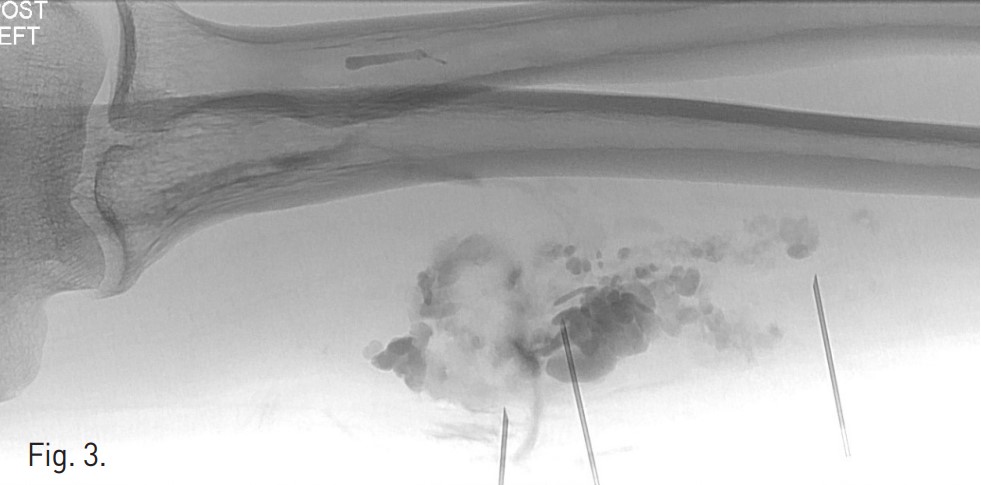
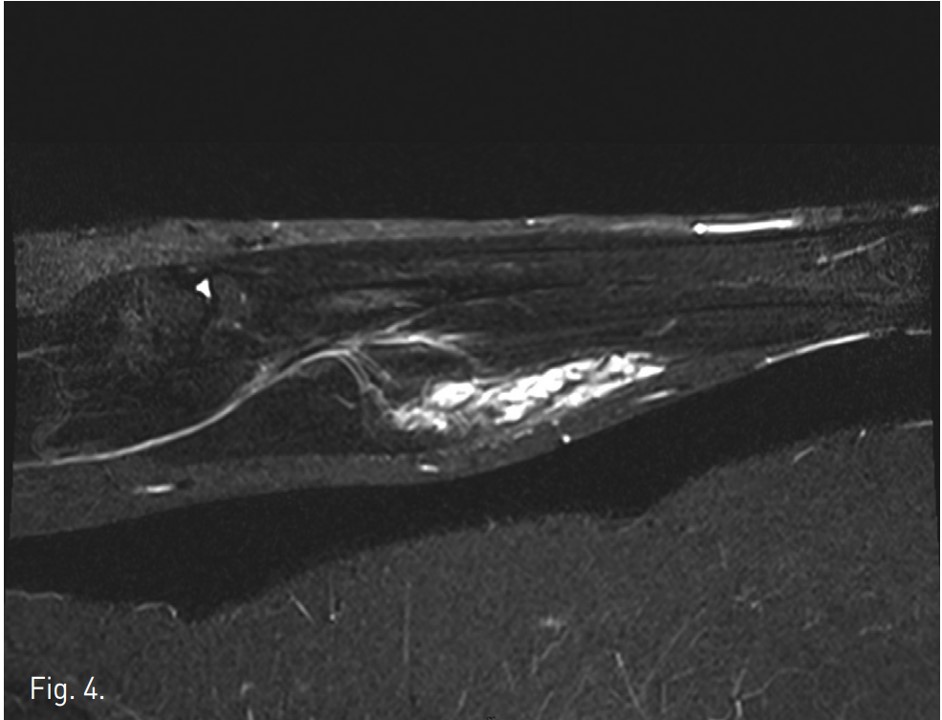
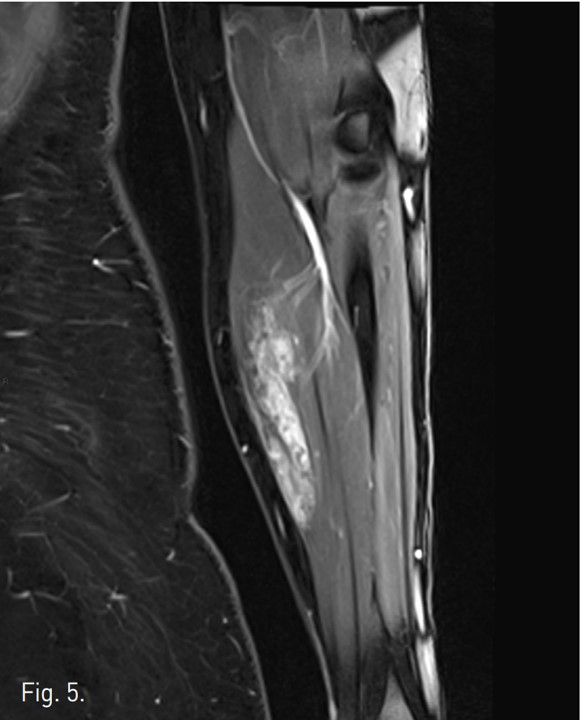
Venography demonstrates dilated, tortuous veins along the medial aspect of the proximal forearm draining into normal veins (Fig. 1). Negative digital subtraction angiography shows filling-defects from displaced contrast material in the vascular malformation during sodium tetradecyl sulfate foam injection (Fig. 2). A native image of the forearm demonstrates stasis of contrast material within the venous malformation after foam sclerotherapy (Fig. 3). T2 STIR imaging shows a 10.3 x 2.5 x 2.3 cm high signal intensity mass centered within the flexor digitorum superficialis consistent with slow-flow vascular malformation. The high signal represents the extent of the vascular malformation as well as post-treatment edema or inflammation (Fig. 4). Post-contra st T1 imaging with fat suppression demonstrates heterogeneous enhancement of the mass with notable areas of low signal representing the areas of thrombosis/sclerosis. The residual irregular enhancement represents postprocedural inflammation. Of note, there are no enhancing serpiginous structures (Fig. 5).
Materials & Methods
The patient was prepped in the usual sterile manner. The venous malformation was accessed with a 21-gauge single wall needle under ultrasound guidance. Hand-injection of contrast material was performed through the needle to identify the anatomy and location of the venous malformation. A tourniquet was applied proximally to further evaluate vascular anatomy. Three percent sodium tetradecyl sulfate (Sotradecol, AngioDynamics, Inc, Queensbury, NY) sclerosing agent was mixed in a 1:1 ratio with air using the Tessari technique. Ten mL of sclerosing foam was injected into the venous malformation under negative digital subtraction angiography (DSA). Five minutes after the injection, venogram demonstrated absence of drainage from the venous malformation into a main proximal venous branch in the forearm. Two additional sites within the venous malformation were accessed and the technique was repeated with the injection of 2.5 mL of sclerosing foam. The needle tracks were embolized with Gelfoam(Pfizer, New York, NY) slurry. The patient was transferred to recovery in stable condition with no complications.
Discussion
Our patient presented with 14 years of symptoms of pain, swelling and decreased range of motion of her left forearm and wrist. MRI demonstrated a low-flow vascular malformation within the flexor digitorum superficialis, which was subsequently found to be a venous malformation. The patient decided to pursue sclerotherapy to alleviate her symptoms. We performed foam sclerotherapy of her venous malformation using 3% sodium tetradecyl sulfate mixed with air in a 1:1 ratio. Follow up visits confirmed that the patient had a positive outcome with improved symptoms. Vascular malformations are categorized as either fast-flow or slow-flow lesions. Fast-flow lesions include arteriovenous malformations, arteriovenous fistulas, and lymphatic arteriovenous malformations (1). Slow-flow lesions include the remainder of vascular malformations, most notably venous malformations, which account for nearly two-thirds of all vascular malformations (2). Lesions with an arterial blood supply are amenable to occlusive embolization or sclerotherapy with absolute alcohol while venous malformations have classically been treated with ethanol (3).
Foam sclerosing agents, including sodium tetradecyl sulfate, have been used in the treatment of vascular malformations (4,5). These agents are beneficial as the air bubbles increase surface contact with the vessel endothelium resulting in improved sclerosing activity at lower doses than conventional ethanol treatment. The lower doses also lead to decreased toxicity from the agent (3).
The percutaneous digital subtraction angiography (DSA) technique we employed has been previously described and found to be effective in treatment of venous malformations(6). The negative DSA technique allows the physician to visualize injection of the sclerosing agent and to ensure that it does not extravasate or enter the normal venous drainage pathways (7). These advantages decrease procedural complications and lead to improved outcomes for patients.
In conclusion, foam sclerotherapy with negative DSA techqnique can be used to safely and effectively treat slow- flow vascular malformations.
References
1. Chim H, Drolet B, Duffy K, et al. Vascular anomalies and lymphedema. Plast Reconstr Surg. 126:55e, 2010.
2. Berg an J, Cheng V. Foam sclerotherapy of venous malformations. Phlebology 2007; 22:299-302.
3. Rockman CB, Rosen RJ, Jacobwitz GR, et al. Transcatheter embolization of extremity vascular malformations: the long-term success of multiple interventions. Ann Vasc Surg 2003;17:417-23.
4. Li L, Zeng XQ, Li YH. Digital subtraction angiography-guided foam sclerotherapy of peripheral venous malformations. AJR 2010; 194:W439-W444.
5. Khandpur S, Sharma VK. Utility of intralesional sclerotherapy with 3% sodium tetradecyl sulphate in cutaneous vascular malformations. Dermatol Surg 2010; 36:340-346.
6. Li L, Feng J, Zeng XQ, et al. Fluoroscopy-guided foam sclerotherapy with sodium morrhuate for peripheral venous malformations: preliminary experience J Vase Surg 2009; 49:961-967.
7. Agid R, Burvin R, Gomori JM. Sclerotherapy for venous malformations using a “negative subtraction” technique. Neuroradiology 2006;48:127-129.
Fig. 1.
Fig. 1. Venography demonstrates dilated, tortuous veins along the medial aspect of the proximal forearm draining into normal veins .
Fig. 2.
Fig. 2. Negative digital subtraction angiography shows filling-defects from displaced contrast material in the vascular malformation during sodium tetradecyl sulfate foam injection.
Fig. 3.
Fig. 3. A native image of the forearm demonstrates stasis of contrast material within the venous malformation after foam sclerotherapy.
Fig. 4.
Fig. 4. T2 STIR imaging shows a 10.3x2.5x2.3 cm high signal intensity mass centered within the flexor digitorum superficialis consistent with slow-flow vascular malformation. The high signal represents the extent of the vascular malformation as well as post-treatment edema or inflammation.
Fig. 5.
Fig. 5. Post-contrast T1 imaging with fat suppression demonstrates heterogeneous enhancement of the mass wi th notable areas of low signal representing the areas of thrombosis/sclerosis. The residual irregular enhancement represents post-procedural inflammation. Of note, there are no enhancing serpiginous structures.
Citations
Citations to this article as recorded by