중심단어
Central venous catheterization, central venous access, thoracic duct, internal jugular vein
한글 초록
중심정맥관의 삽입과정 중 동맥성 출혈 또는 기흉과 같은 다양한 합병증이 발생할 수 있다. 매우 드물게 림프관의 손상에서 비롯되는 림프액 유출이 발생할 수 있다. 37세 여자 환자에서 정맥포트삽입 과정 중 가슴관 손상이 발생한 증례를 보고 한다.
영문 초록
Lymphatic injury is a rare complication of central venous catheterization. We report a case of thoracic duct injury that occurred during placement of an intravenous chemoport in a patient with breast cancer.
Introduction
Central venous catheterization is one of the most commonly performed procedures in medicine. The procedure is technically simple and can be performed either at bed side or under ultrasound with or without fluoroscopy. The use of both ultrasound and fluoroscopy which are both available in the angiography suite decreases the likelihood of catheter misplacement and complications that result thereof such as inadvertent arterial injury and pneumothorax [1]. Herein, we report a rare care of thoracic duct injury during placement of a central venous chemoport.
Case report
증례
37세/여자
임상소견
A 37-year-old female with right-sided breast cancer was referred to our department for placement of a central venous chemoport. Before admission, she underwent the right breast resection and dissection of ipsilateral axillary lymph nodes.
진단명
Breast cancer, referred for chemoport placement.
시술방법 및 재료
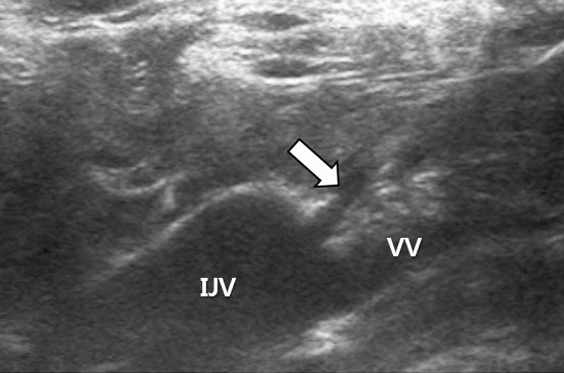
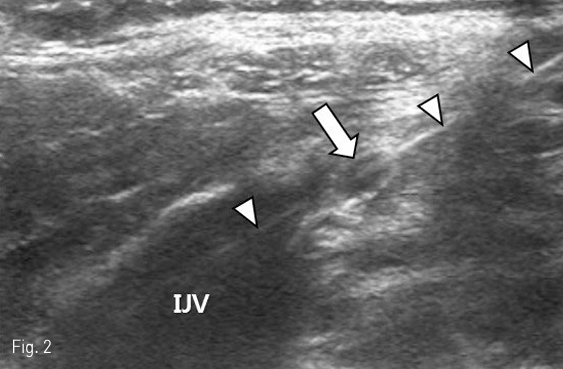
After sterile preparation of the neck and left chest wall, local anesthesia of the skin and subcutaneous tissue overlying the left internal jugular vein was performed by injecting lidocaine 2%. The left internal jugular vein was then punctured with a 19-guage needle under ultrasound guidance and a 0.035-inch guide wire with a J-tip was passed through the needle bore and directed into the right atrium under fluoroscopy. After creating a subcutaneous pocket in the left subclavian fossa which would harbor the infusion port, a tunneling device that attached to the infusion catheter was advanced through the subcutaneous layer from the pocket towards the venous access site. Following the tunneling maneuver, a stream of “milky”fluid was seen to spill out of the skin at the point of venous access (Fig. 1). This fluid was immediately recognized to be chyle and ultrasound was used to reveal the course of the guide wire traversing the cervical portion of the thoracic duct (Fig. 2). Before foregoing aggressive intervention, conservative management was attempted by manual compression after guide wire removal. In line with our expectations, stasis of chyle spillage was achieved with light compression for ten minutes. In order to complete the chemoport placement procedure, a new access was created in the left internal jugular vein, albeit a little more cephalad to the original puncture site. The chemoport was finally placed without complication.
추적관찰
The patient was uneventfully discharged three days later during which time she was observed by physical examination and serial chest radiography for possible delayed complication.
Fig 1
Spillage of chyle (arrowheads) can be seen at the site of venous access.
Fig 2
Ultrasound demonstrating the thoracic duct (arrow) between the left internal jugular vein (IJV) and vertebral vein (VV). A guide wire (arrowheads) penetrating the thoracic duct is noted.
Fig 2
Ultrasound demonstrating the thoracic duct (arrow) between the left internal jugular vein (IJV) and vertebral vein (VV). A guide wire (arrowheads) penetrating the thoracic duct is noted.
고찰
The true incidence of lymphatic injuries during central venous catheterization is unknown owing to the rarity of such complications. This is reflected by the scarcity of literature which is limited to isolated case reports [2-6]. Although fluid analysis was not performed in our case, the characteristic “milky”appearance of chyle was suggestive of thoracic duct injury and this was correlated on ultrasound. The thoracic duct is the largest lymphatic vessel in the body and drains almost of the body’s lymph. It is the common trunk for all the lymphatic vessels of the body, excepting those on the right side of the head, neck, and thorax, the right upper extremity, right lung, right side of the heart, and the convex surface of the liver. The thoracic duct usually terminates at the junction of the left internal jugular vein and left subclavian vein, a site that is commonly referred to as the jugulovenous angle [7,8]. In our case, ultrasound demonstrated the guide wire which had penetrated the cervical portion of the thoracic duct. The cervical portion of the thoracic duct is an anatomical landmark where the thoracic duct passes up and over between the left internal jugular and vertebral veins before it joins the jugulovenous angle. High-resolution ultrasound imaging with linear probes have been shown to be useful for visualizing the portion of the thoracic duct [9]. Although the use of ultrasound guidance has been shown to reduce the risk of complications that potentially occur during central venous catheterization, the presence of the thoracic duct may be overlooked without special attention. With regard to left-sided central venous catheterization, scrutiny during ultrasound guidance is mandatory, not only to avoid vascular complications, but also lymphatic injury. Interventional radiologists who commonly perform ultrasound-guided venous access in the neck region should be familiar with the anatomy of the thoracic duct and how it appears under ultrasound.
참고문헌
1. Nayeemuddin M, Pherwani AD, Asquith JR. Imaging and management of complications of central venous catheters. Clin Radiol 2013; 68: 529-544
2. Beljaars GH, Van Schil P, De Weerdt A, Suys B, Wojciechowski M, Jorens PG. Chylothorax, an unusual mechanical complication after central venous cannulation in children. Eur J Pediatr 2006;165: 646 647
3. Barnacle AM, Kleidon TM. Lymphatic leak complicating central venous catheter insertion. Cardiovasc Intervent
Radiol 2005; 28: 839-840
4. Kwon SS, Falk A, Mitty HA. Thoracic Duct Injury Associated with Left Internal Jugular Vein Catheterization: Anatomic Considerations. J Vasc Interv Radiol 2002;13: 337-339
5. Chandiraseharan VK, Malathy AR. An unusual 86 complication of central venous catheterization. CHRISMED Journal of Health and Research, 2015;2: 276-278
6. Teichgraber UK, Nibbe L, Gebauer B, Wagner HJ. Inadvertent puncture of the thoracic duct during attempted central venous catheter placement. Cardiovasc Intervent Radiol. 2003; 26: 569-571
7. Phang K, Bowman M, Phillips A, Windsor J. Review of thoracic duct anatomical variations and clinical implications. Clin Anat. 2014;27: 637-644
8. Kinnaert P. Anatomical variations of the cervical portion of the thoracic duct in man. J Anat 1973;115:45-52
9. Seeger M, Bewig B, Günther R, et al. Terminal Part of Thoracic Duct: High-Resolution US Imaging. Radiology 2009;252:897-904
Citations
Citations to this article as recorded by